It’s probably happened to you a million times while flipping through your notes: the handwriting is barely legible, full of jargon you may have already forgotten, and doesn’t give you a clear picture of what happened or what issues still need to be addressed. Sound familiar?
Most medical practitioners have been there, which is why good medical documentation is absolutely essential for providing quality care and avoiding mistakes.
But, it’s a skill that takes practice to master. Don’t worry, though!
In this article, we’ll cover what medical documentation is, why it matters, and give you some tips and tools to ace it every single time.
We’ll go over:
- What is medical documentation and why does it matter?
- What’s the use of medical documentation?
- Why is medical documentation used, anyway?
- What should a good set of medical documents include?
- Nurses vs doctors: A side-by-side medical documentation comparison
Let’s get started!

What is medical documentation and why is it important?
In a nutshell, we refer to medical documentation as the written records of a patient's medical care.
It includes notes from doctors, nurses, and other healthcare professionals about a patient's condition, treatment, and progress.
What is medical documentation used for?
There are several purposes for comprehensive medical documentation, and they are:
- They help maintain ongoing care. Medical documentation allows different healthcare providers to access a patient's history, understand past treatments, and make informed decisions about future care. This type of seamless transition between providers is a necessity for effective and efficient patient care, especially in complex cases that need multidisciplinary attention.
- For legal protection: These records also serve a legal purpose, providing a factual account of the care provided.
In the event of legal inquiries or even all-out disputes, medical documentation can protect healthcare providers by demonstrating adherence to standards of care and informed consent.
Medical documentation also offers a clear defense against malpractice claims, showcasing the rationale behind clinical decisions and interventions.
- It’s all about quality and safety: Well-maintained medical records contribute to patient safety and the quality of care. In essence, they enable healthcare professionals to identify potential issues, such as allergies or adverse reactions, and prevent medical errors. Additionally, thorough documentation supports quality improvement initiatives by allowing for the review and analysis of clinical outcomes, which guides strategies to enhance care delivery.
- Communication matters: Medical documentation is also important for facilitating communication between team members.
It serves as a central point of reference for discussions about patient care, which guarantees that all team members are kept in the loop and aligned in their approach.
- It’s important for reimbursement: In the context of insurance and billing, medical documentation plays a huge role in reimbursement processes.
How? By providing the necessary evidence to support claims for medical services rendered, detailing the care provided, and justifying the costs incurred.
If healthcare providers need to receive appropriate compensation from insurance companies, accurate documentation is absolutely necessary.
- It matters for research and education: Medical records also make a difference by contributing to the advancement of medical knowledge and the development of new treatments.
They offer a nearly bottomless source of data for clinical studies, helping to identify trends, outcomes, and areas for improvement.
Further, medical documentation is a critical tool for educational purposes, allowing students and trainees to learn from real-world cases.
What should medical documentation include?
Reliable medical documentation goes way beyond scribbling notes with barely legible handwriting. There’s a method to the madness, called SOAP.
It stands for:
- Subjective: This is where you document the patient’s symptoms, medical history, and complaints in their own words. Write down information about their lifestyle, family medical history, medications, allergies, and social history.
- Objective: Now, it’s time to note your objective observations during the physical exam. This includes things like vital signs, test results, and any physical findings. Remember to be detailed and accurate.
- Assessment: Provide your professional analysis of the patient’s condition and diagnoses based on the subjective information and objective data. After, list any differential diagnoses you are considering.
- Plan: Outline the plan of care including any tests, procedures, medications, therapies, or follow-ups needed. Also, provide any specific details for all recommendations and make sure to note if the patient understands and agrees with the plan.
Following the SOAP format is part and parcel of providing solid and reliable medical notes.
Also, don’t forget to date and sign all entries, use approved medical abbreviations, and avoid vague or ambiguous language.
Finally, proofread carefully to make sure that there are no spelling, grammar, or punctuation errors before entering the record into the EHRs (Electronic Health Records).
Medical documentation by healthcare profession - nurses vs doctors
Medical documentation is equally important across all medical professions. However, the focus and level of detail can differ between professions.
Let’s take a look at an example comparison:
Nurses
Nurses typically document more frequently, recording vital signs, input/output, wound care, ADLs, and other routine care.
Nurses set out to capture the patient’s condition and response to treatments, which means they typically note subjective symptoms described by the patient and objective observations.
The medical documentation should be clear, concise, and include:
- Patient complaints and symptoms
- Vital signs, test results, and observations
- Medications administered and patient response
- Treatments, procedures, ADLs, and education provided
- Plan for ongoing care
These nurse notes give doctors a glimpse into the patient’s status between rounds so they have the full picture when assessing the patient.
Doctors
Doctors have a big focus on diagnostic and therapeutic decision-making. Therefore, they document medical history, examination findings, differential diagnoses, test orders, and treatment plans.
Doctors are looking to justify diagnoses, treatment plans, and discharge.
So, their notes should capture:
- Medical history and symptoms as described by patient
- Physical exam and test findings
- Differential diagnoses and final diagnosis
- Orders for medications, tests, consults, and procedures
- Treatment plans and patient education
- Prognosis and follow-up plan
As we mentioned above, doctors depend on nursing documentation to understand how the patient has progressed and responded since the last visit.
Together, these nursing and medical notes paint a complete picture of the patient's hospital stay and the care provided.
Summing up
Medical documentation is a tedious, painstaking process, but it's essential for providing quality care and protecting patients and providers.
By following best practices like SOAP - focusing on relevant details, keeping it simple and clear will help you document efficiently while covering all the bases. Even if it takes time, the alternative is providing worse care, and we know that’s not a real option!
Next steps
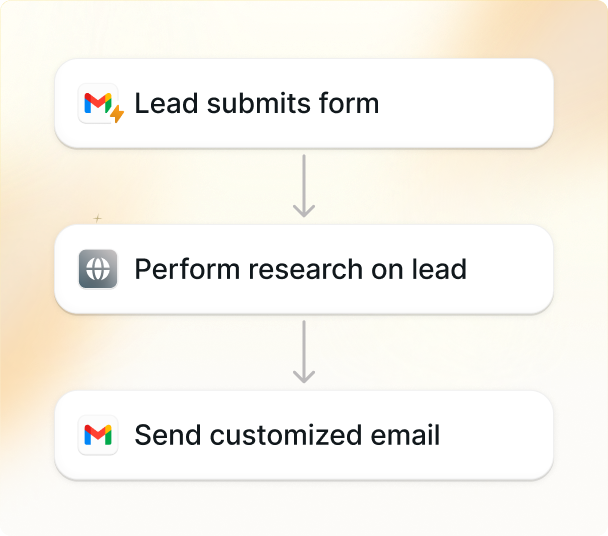
Are endless mountains of paperwork robbing you of valuable patient face-time? Lindy’s cutting-edge superhuman AI is here to take care of your medical documentation.
- 80% reduction in charting time: Get 8 hours per week back for what matters most – your patients.
- You save money, and earn more: $20,000-$45,000 increased annual earnings per doctor (clinician studies).
- Beyond human capabilities: Medically tuned AI picks up on medical terms and shorthand and ensures your documentation is flawless, secure, and HIPPA compliant.
- No more time-consuming software: Seamlessly integrate Lindy with your existing systems (like Zoom or your EMR) and add customizable templates into your workflow.
Don’t take our word for it. Try out Lindy for free and see why thousands of practitioners are charting with Lindy.
Explore AI-powered, HIPAA-compliant Medical Dictation with Lindy