SOAP notes can be a real pain in the brain. But writing effective psych notes doesn't have to drive you up a wall.
In this article, we'll walk you through the SOAP method, provide examples of solid psychiatry notes, give some proven tips to optimize your time — and throw a technological bone your way.
We’ll go over:
- What is a psychiatry note and why would you even take them? (With details about the SOAP method)
- How do you take SOAP notes in psychiatry?
- Two examples of psychiatry SOAP notes
- How do you optimize your note-taking?
- FAQs
Let’s get started!

What is a psychiatry note and why do you take them?
Psychiatry notes provide a written record of a patient’s treatment and progress.
They help clinicians keep track of symptoms, medications, side effects, and whether that weird rash was from the Abilify or the Lamictal (just kidding...kind of).
The SOAP note is the clinician's way of organizing your information:
- The S stands for Subjective and includes your description of how a patient is doing and any concerns they may want to discuss.
- The O is for Objective and refers to a clinician’s observations about a patient’s appearance, behavior, and cognitive functioning.
- The A stands for Assessment, a clinician’s professional opinion about what's going on based on the S and O.
- The P is the Plan, which outlines steps for treatment. This may include medication changes, referrals to other doctors, or recommendations for therapy. SOAP notes provide consistency and help make sure patients get tip-top care from visit to visit.
Also, while notes are primarily for the patient’s benefit, insurance companies and healthcare systems also require them.
In today's world, if it's not documented, it didn't happen. These notes also need to abide by strict confidentiality guidelines.
(They don’t cover gossiping during coffee breaks, thankfully).
How do you take SOAP notes in psychiatry?
The SOAP method is tried and true, so even if you’re groaning at the idea of having to write things down after a long, grueling day, take heart! We’ll show you how to get it right so you don’t have to spend the night scribbling away.
Let’s get started:
- Subjective
This is where you get into your patient’s head. Ask open-ended questions about how they’re feeling and any symptoms they’ve noticed; you know the deal. Really listen and write down what they say word-for-word, or at least get the gist of it as much as possible. You’ll thank us later.
- Objective
Now it’s time for you to put on your detective hat. Note any observations about the patient’s appearance, behavior, mood — anything factual you pick up on. Be detailed but neutral. This is the time to leave personal opinions at the door!
- Assessment
Here’s why you get paid the big bucks: Making a diagnosis! Review your subjective and objective findings and determine what’s really going on with your patient. Refer to the DSM if you need to, there’s no shame in that. Come up with a diagnosis and thoroughly record how you came to your conclusion.
- Plan
Last but not least, map out a treatment plan. Will therapy or medications be better? What interventions will you try? How often will you see the patient? Lay out the next steps to getting them back on track.
Examples of psychiatry notes
Now it’s time to put that knowledge into action with a couple of examples.
Psychiatry note example #1
Major depressive disorder with suicidal ideation:
- S: Patient is a 45-year-old female presenting with depressed mood, anhedonia, and persistent suicidal thoughts. She reports feeling "empty and worthless" for the past several months, with worsening symptoms in the past two weeks. Describes difficulty sleeping, decreased appetite, and significant fatigue.
Patient admits passive suicidal ideation of wanting to "go to sleep and not wake up," with occasional thoughts of overdosing on her medications. Denies a specific plan or intent to harm herself.
- O: Patient appears disheveled, with slumped posture and minimal eye contact. Affect is flat and she speaks in a soft, monotone voice. Thought content reveals significant self-deprecation and pervasive hopelessness. Patient's insight is limited, as she believes her situation will not improve. No overt signs of psychosis.
- A: Major Depressive Disorder, single episode, severe.
Suicidal ideation, passive, without intent or plan.
- P: Initiate escitalopram 10mg daily, titrate up as tolerated.
Schedule urgent outpatient psychotherapy referral specializing in Cognitive Behavioral Therapy (CBT).
Implement safety plan: Restrict access to lethal means, increase frequency of social contact (appoint family member to stay with patient if possible).
Reassess in 1 week, sooner if symptoms acutely worsen. Consider inpatient admission if suicidal ideation escalates or patient cannot maintain safety at home.
Sounds like too much? Thankfully, that’s on the longer end of the spectrum, and — due to the gravity of this case — far more detailed than what you will typically write in your day-to-day psychiatry SOAP notes.
The following example will be much more representative of daily interactions, such as in a follow-up appointment:
Note #2
- S: Patient is a 38-year-old female with a diagnosis of generalized anxiety disorder (GAD). Reports some improvement in anxiety since starting sertraline but continues to experience intrusive worries about her health and frequent muscle tension.
- O: Patient appears slightly tense, with occasional fidgeting. Speech is normal in rate and volume. Affect is congruent with mood, with some mild anxiousness evident. Thought processes are linear and logical. Denies suicidal or homicidal ideation.
- A: Generalized Anxiety Disorder, moderate, with partial response to medication.
- P: Increase sertraline to 100mg daily.
Continue weekly psychotherapy sessions focused on cognitive restructuring.
Teach patient basic relaxation techniques (e.g., deep breathing, progressive muscle relaxation).
Follow-up in 4 weeks to reassess medication response and symptom severity.
How do you optimize for time with psychiatry notes?
Optimizing your time with psychiatry notes is pretty much synonymous with avoiding burnout.
Here are a few tips to shorten the time you spend on notes without sacrificing quality:
- Keep it brief. When describing the patient’s symptoms and condition, stick to the essentials. There’s no need to recount every detail of their childhood or list every symptom they’ve ever had. Focus on what’s relevant to their current treatment plan.
Use bulleted lists and shorthand when possible. If another clinician gets the case, they will understand.
- Reuse and recycle. If you find yourself writing the same instructions or observations for multiple patients, save time by creating template notes you can reuse and modify as needed. Have a standard template for common conditions like depression or anxiety that includes typical symptoms, medications, and follow-up plans. You can then customize the details for each patient.
- Dictate when you can. Speaking your notes aloud using AI-powered dictation software is way faster than typing them out. After a session, speak aloud your observations, assessments, and plans for patient care. Then review and modify the transcribed notes as needed (AI will even give you nifty suggestions).
With practice, dictation can become second nature and significantly cut down the amount of time spent on notes.
- Keep a schedule. Try to complete your notes as soon as possible after seeing each patient while the details of your discussion are still fresh in your mind. If you fall behind, you’ll end up spending more time trying to remember specifics. You’ll also avoid the dread of facing a mountain of unwritten notes at the end of the week.
Even sticking to a regular schedule of completing a set number of notes each day can help make the process feel like less of a chore.
Psychiatry note FAQs
How long do I have to finish my notes?
The general rule of thumb is to complete notes within 24 hours of seeing the patient. Some places may require notes within a shorter timeframe, so check with your organization’s policy. The key is to be timely while also being thorough. No pressure!
Can I copy and paste between patient notes?
While recycling content may save time, it’s not advisable for psychiatry notes. Each patient and session is unique, so notes should reflect that. Generic or copied content could compromise care and won’t provide an accurate record of the patient’s condition and progress. It’s best to create customized notes for each patient at each visit.
Do I have to write in SOAP format?
SOAP (Subjective, Objective, Assessment, Plan) is a common format for medical notes, but it’s not required for psychiatry. Some psychiatrists prefer different formats they find more intuitive for mental health, e.g. chronological narratives or problem-oriented notes. The most important thing is that your notes are organized, comprehensive, and help demonstrate medical necessity for treatment.
Summing up
That’s psychiatrist notes demystified for you.
You now possess the power to channel your inner Freud and scribble down those SOAP notes like a pro.
Keep it simple and focus on the facts. Before you know it, you'll be cranking out therapy write-ups faster than you can say, "Tell me about your childhood."

Next steps
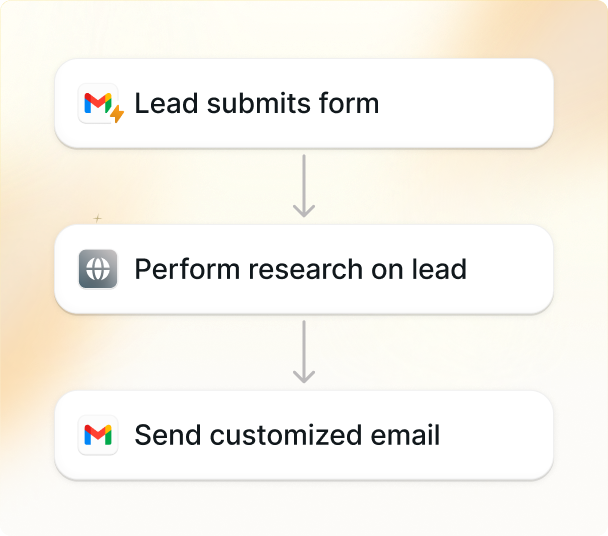
Upgrade your practice with Lindy, the AI assistant built for mental health professionals.
Here's how Lindy streamlines your psychiatric documentation:
- Ready-made EHR integration: Lindy works seamlessly with your existing workflow, especially common platforms like SimplePractice. It's about efficiency, not adding complexity.
- Specialized for psychiatry: Lindy's AI is trained on psychiatric terminology and concepts, guaranteeing a 99%+ accurate transcription of diagnoses, mental status observations, and treatment plans.
- Dictate directly into SOAP format: After sessions, simply speak your notes. Lindy intelligently converts your dictation into the appropriate SOAP note sections, saving you over 2 hours of data entry per day.
- Review and edit easily: Make any necessary adjustments to your notes directly within your EHR, maintaining your usual workflow — only faster and 90% more accurate.
- Supports trainees and supervisors: Lindy can archive dictations of training sessions, facilitating feedback and aligning with the needs of training programs.
- Security is peace of mind: Lindy adheres strictly to HIPAA and PIPEDA standards, for maximum patient confidentiality. Data remains protected and is never used for any other purpose.
- Faster notes, more focus: Dictation with Lindy slashes patient documentation time by 80%, giving you more time for client care or much-needed self-care.
















.png)
.png)
.png)
%20(1).avif)